Diseases of the circulatory system are among the main causes of mortality in each of the EU countries (as shown in Table 1): in 2021, they accounted for more than half of all deaths in Bulgaria and Romania. By contrast, less than a quarter of all deaths in France, Denmark, the Netherlands, Belgium and Luxembourg were caused by diseases of the circulatory system; France had the lowest share, at 20.9%.
The largest gaps between the sexes in relation to the share of people dying from diseases of the circulatory system were recorded in the 3 Baltic countries as well as Slovenia, Romania and Croatia. In these EU countries, the proportions of females dying from diseases of the circulatory system in 2021 were between 9.7 and 14.5 percentage points (pp) higher than those for males; these were the only EU countries to report an imbalance in excess of 9.0 points. There were only 4 EU countries where a higher proportion of males died from diseases of the circulatory system compared to females: in Denmark and Finland, the shares of male deaths were, respectively, 1.6 and 1.0 pp higher than those for females; smaller differences were observed in Sweden and Ireland. In Cyprus, the shares were the same for males and for females.
Malta recorded the narrowest gender difference in standardised death rates for diseases of the circulatory system
Standardised death rates are calculated as a weighted average of age-specific death rates and therefore improve comparability both over time and between countries. The EU’s standardised death rate for diseases of the circulatory system was 343.4 deaths per 100 000 inhabitants in 2021, with the rate for males some 1.4 times as high as that for females. In the same year the standardized death rate for cancer in the EU was 235.
Standardised death rates for diseases of the circulatory system were systematically higher for males than for females in 2021 across all of the EU countries, although the differences between the sexes were relatively low compared with many other causes of death. The lowest absolute difference between males and females for standardised death rates for diseases of the circulatory system was recorded in Malta, at 54 deaths per 100 000 inhabitants; the next smallest differences (around 80 deaths per 100 000 inhabitants) were reported in the Netherlands and Cyprus. The largest difference was recorded in Bulgaria (478 deaths per 100 000 inhabitants).
Table 1 shows that deaths from diseases of the circulatory system become more common at advanced ages. While this was true for the vast majority of causes of death, the standardised death rate for diseases of the circulatory system among those aged 65 years and over in the EU in 2021 was 37 times as high as the standardised death rate for people aged less than 65 years; this can be compared with the same ratio for all causes of death, where the standardised death rate for those aged 65 years and over was 21 times as high as for people aged less than 65 years. Note that the risk of females dying from diseases of the circulatory system before the age of 65 years was particularly low.
Within the EU as a whole, standardised death rates for males were consistently higher than those for females for all forms of diseases of the circulatory system
A more detailed analysis of causes of death for diseases of the circulatory system is presented in Table 2. EU standardised death rates for males in 2021 were higher than those for females for each of the 6 causes of death presented. For ischaemic heart diseases (International Classification of Diseases, 10 revision (ICD-10) codes I20 to I25), the standardised death rate for males in the EU was 1.9 times as high as the corresponding rate for females. The difference between the sexes was less marked for other heart diseases (ICD-10 codes I30 to I51), cerebrovascular diseases (ICD-10 codes I60 to I69) and other diseases of the circulatory system (the remainder of ICD-10 codes I00 to I99, not elsewhere covered).
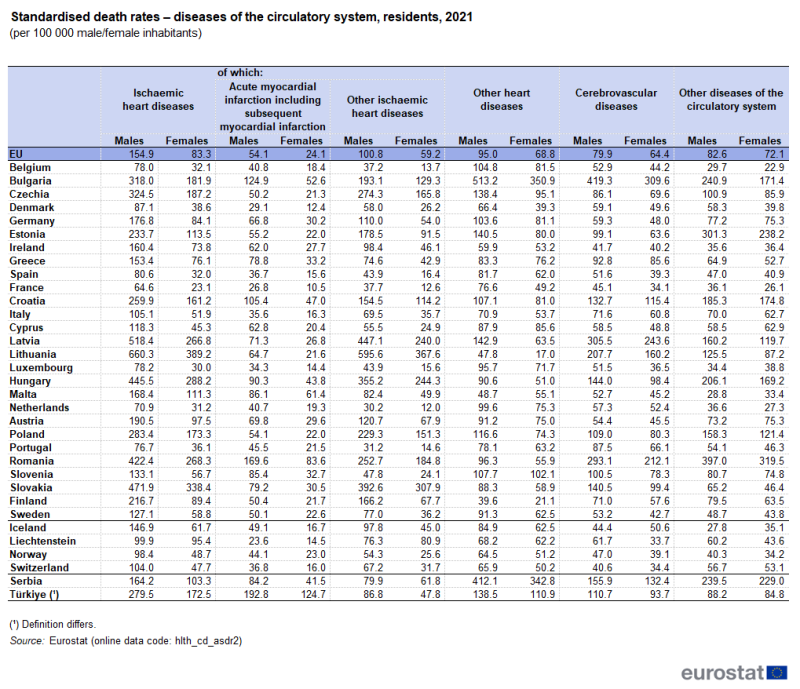 Table 2: Standardised death rates – diseases of the circulatory system, residents, 2021
Table 2: Standardised death rates – diseases of the circulatory system, residents, 2021
(per 100 000 male/female inhabitants)
Source: Eurostat (hlth_cd_asdr2)
Some of the highest standardised death rates for ischaemic heart diseases were recorded in 2 of the Baltic countries: Lithuania had the highest rate in 2021 for males (660.3 per 100 000 male inhabitants) and for females (389.2 per 100 000 female inhabitants), followed by Latvia and Slovakia for males, and Slovakia and Hungary for females. By contrast, the lowest standardised death rates for males were recorded in France, followed by the Netherlands and Portugal. For females the lowest standardised rates were recorded in France followed by Luxembourg and Netherlands.
The standardised death rate for cerebrovascular diseases in Bulgaria was 9.1 times as high as the rate in France
In 2021, the highest standardised death rates for cerebrovascular diseases were recorded in Bulgaria, Latvia, Romania and Lithuania. By contrast, the lowest rates were recorded in France and Ireland. As for all diseases of the circulatory system, there were large variations across the EU countries in standardised death rates for cerebrovascular diseases in 2021, with the death rate in Bulgaria (where the highest rate was recorded) 9.1 times as high as that in France (where the lowest rate was registered).
Cardiovascular healthcare
Changes in the number of deaths associated with diseases of the circulatory system may occur for a variety of reasons, including preventive measures such as, among others, lifestyle changes in the population (for example, a reduction in the number of smokers), the improvement of screening for risk factors, as well as new surgical procedures and forms of medication.
The number of in-patients with diseases of the circulatory system discharged from hospitals across the EU was 8.6 million in 2021
Hospital discharges of in-patients treated for diseases of the circulatory system show a very large variation across the EU countries. While absolute figures for discharges are clearly linked to the number of inhabitants in each country, the level of discharges may, among other influences, also reflect the incidence of each disease and differences in healthcare systems, for example, the balance between day care and in-patient treatment, as well as the availability of surgeons, hospital beds, or emergency interventions and care facility at hand. In 2021, there were 8.6 million in-patients with diseases of the circulatory system discharged from hospitals across the EU (2020 data for Malta; no recent data for Denmark, Greece or Luxembourg).
Bulgaria recorded the highest ratio per inhabitant of hospital discharges for in-patients with diseases of the circulatory system
Bulgaria and Germany both reported more than 3 000 in-patient discharges per 100 000 inhabitants among those treated for diseases of the circulatory system in 2021 (see Figure 1). Malta (2020 data), Ireland and Portugal recorded the lowest ratios; they were the only EU countries with fewer than 1 100 discharges per 100 000 inhabitants.
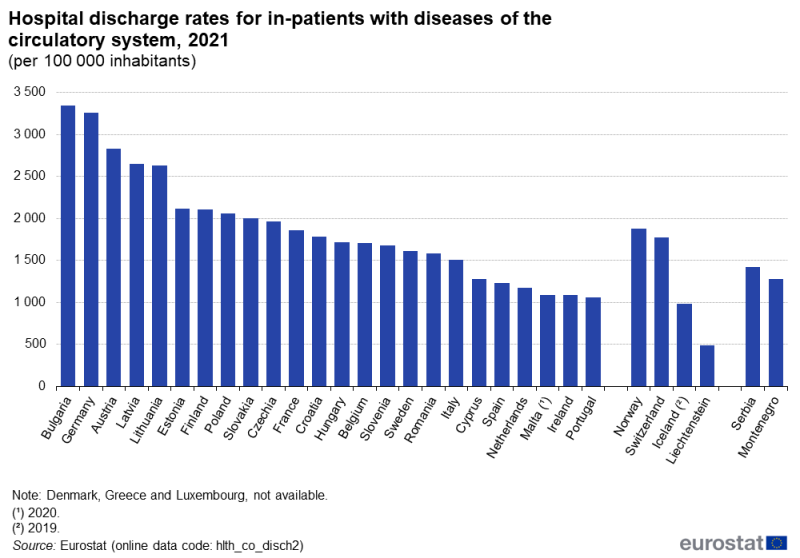 Figure 1: Hospital discharge rates for in-patients with diseases of the circulatory system, 2021
Figure 1: Hospital discharge rates for in-patients with diseases of the circulatory system, 2021
(per 100 000 inhabitants)
Source: Eurostat (hlth_co_disch2)
In 2021, across the EU, in-patients with diseases of the circulatory system (ICD-10 codes I00 to I99) spent a total of 69 million days in hospital (2020 data for Malta; no recent data for Denmark, Greece or Luxembourg). By far the highest share – more than a third of the total (34.9%) – was accounted for by in-patients in Germany, while Italy (12.1%) and France (11.6%) were the only other EU countries recording double-digit shares [1].
In-patients with diseases of the circulatory system in Hungary spent, on average, 11.1 days in hospital per stay
When patients are treated for a disease of the circulatory system, they tend to spend a relatively lengthy period of time in hospital, reflecting the seriousness of some of these conditions. Table 3 presents an analysis of the average length of hospital stays for in-patients treated for a disease of the circulatory system in 2016 and 2021. The average length of stay in 2021 ranged from 4.1 days in Bulgaria up to 11.1 days in Hungary. Relatively lengthy average stays in hospital for in-patients treated for diseases of the circulatory system were also recorded in Austria and Estonia (10.4 and 10.3 days, respectively).
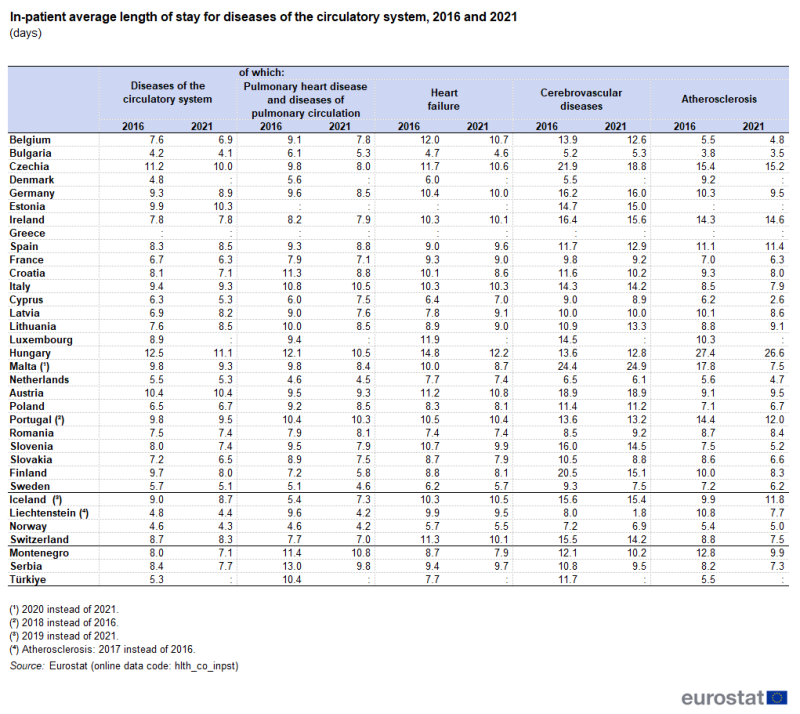 Table 3: In-patient average length of stay for diseases of the circulatory system, 2016 and 2021
Table 3: In-patient average length of stay for diseases of the circulatory system, 2016 and 2021
(days)
Source: Eurostat (hlth_co_inpst)
Among the 24 EU countries for which data are available (see Table 3), a majority (17) recorded a fall between 2016 and 2021 in the average length of a hospital stay for people who were treated for a disease of the circulatory system. The largest decrease – 1.7 fewer days in hospital – was recorded in Finland, while decreases of 1.4 days and 1.2 days, respectively, were recorded in Hungary and Czechia; these were the only EU countries to record falls of more than 1.0 days. By contrast, the average length of a hospital stay for people who were treated for a disease of the circulatory system rose by 1.3 days and 0.9 days in Latvia and Lithuania, respectively, with smaller increases in Estonia, Spain and Poland; there was no change in Ireland and Austria.
Table 3 also provides a more detailed analysis of the average length of hospital stays for in-patients treated for 4 different types of circulatory disease. On average, in both 2016 and 2021, in-patients with cerebrovascular diseases (ICD-10 codes I60 to I69) spent the highest number of days in hospital, followed by those treated for heart failure (ICD-10 code I50) or atherosclerosis (ICD-10 code I70). While it could be assumed from Table 3, that patients with more serious conditions require a longer stay in hospital, this is not always the case. For example, the average length of stay for acute myocardial infarction, (also known as heart attack) (ICD-10 codes I21-I22), in 2021, ranged from 9.1 in Lithuania to 3.9 in Sweden; only Latvia was above this range with 16.3 days. On average, patients with acute myocardial infarction spent fewer days in hospital than for the circulatory diseases presented in Table 3.
Transluminal coronary angioplasty was a common form of intervention for patients treated for cardiovascular diseases
Table 4 provides an overview of the rates (number of surgical operations and procedures conducted, both for inpatients and day cases, in hospitals per 100 000 inhabitants) for 2 procedures related to cardiovascular diseases. The more common of the 2 was transluminal coronary angioplasty, which is a non-surgical procedure used to treat coronary arteries that have narrowed; a deflated balloon is fed through blood vessels until it reaches the site of the blockage before inflating the balloon to open up the artery (allowing blood to flow normally).
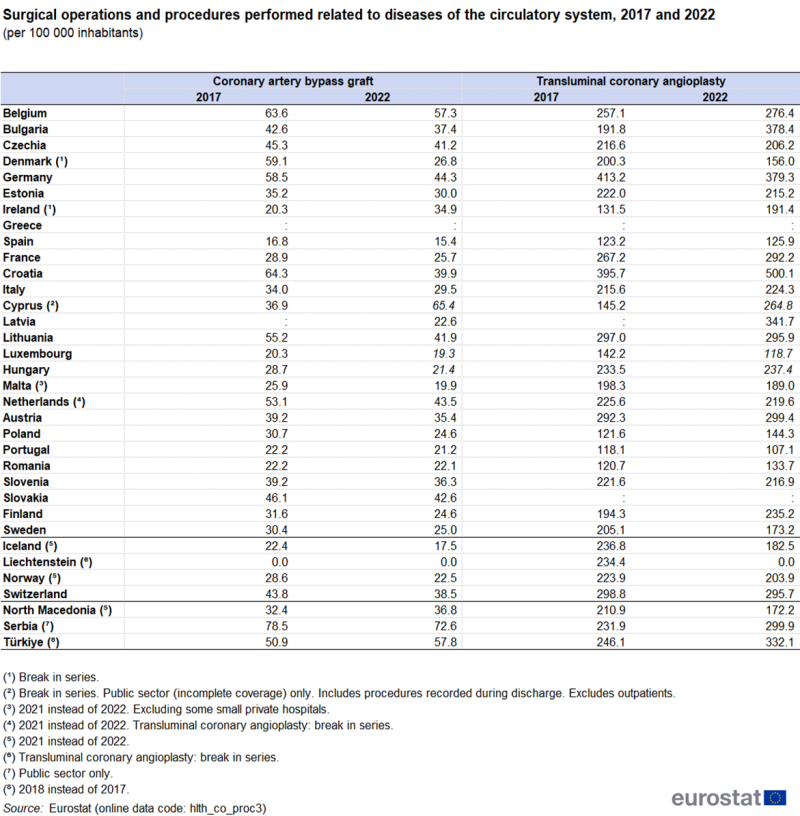 Table 4: Surgical operations and procedures performed related to diseases of the circulatory system, 2017 and 2022
Table 4: Surgical operations and procedures performed related to diseases of the circulatory system, 2017 and 2022
(per 100 000 inhabitants)
Source: Eurostat (hlth_co_proc3)
A relatively common operation for patients treated for cardiovascular diseases was a bypass anastomosis for heart revascularisation – also referred to as a coronary artery bypass graft or heart bypass. This is a surgical procedure whereby arteries to the heart are replaced by blood vessels from another part of the body. In 2022, there were 136 100 heart bypass operations conducted across the EU (2021 data for Malta and the Netherlands; no recent data for Greece), over 26 000 operations lower than in 2017. In relative terms, the number of heart bypasses per 100 000 inhabitants decreased in all but 2 EU countries (Ireland and Cyprus; note there in a break in series) between 2017 and 2022.
Germany recorded the highest number of operations (37 100) and had the 3rd highest frequency when taking account of population size (44.3 per 100 000 inhabitants), behind Cyprus (65.4 times per 100 000 inhabitants; data for the public sector only) and Belgium (57.3 times per 100 000 inhabitants). This procedure was least common in Spain, where it was performed on average 15.4 times per 100 000 inhabitants.
317 800 coronary angioplasties were conducted in Germany in 2022
Across the 25 EU countries for which data are available (2021 data for Malta and the Netherlands; no recent data for Greece or Slovakia), there were 1.06 million transluminal coronary angioplasty procedures conducted in 2022. This was over 3 500 procedures higher than in 2017. In relative terms, the number of transluminal coronary angioplasty procedures per 100 000 inhabitants increased in 13 EU countries. The highest increase was recorded in Bulgaria, where the number of transluminal coronary angioplasty procedures increased by 189.7 procedures per 100 000 inhabitants between 2017 and 2022. The biggest decrease was recoded in Denmark; down 44.3 procedures per 100 000 inhabitants.
Germany accounted for around 30% (317 800) of the procedures that took place in the EU in 2022, which was considerably higher than in any of the other EU countries; France and Italy were the only other EU countries to report in excess of 100 000 procedures. Not only did Germany report the largest number of such operations, but also the 2nd highest ratio when taking account of the size of its population (see Table 4): 379.3 transluminal coronary angioplasty procedures were performed in Germany per 100 000 inhabitants. The highest ratio was 500.1 per 100 000 inhabitants in Croatia. This procedure was least common in Portugal where it was conducted 107.1 times per 100 000 inhabitants, while relatively low ratios were also recorded in Luxembourg, Spain and Romania.
Source data for tables and graphs
Data sources
Key concepts
An in-patient is a patient who is formally admitted (or ‘hospitalised’) to an institution for treatment and/or care and stays for a minimum of 1 night in the hospital or other institution providing in-patient care.
A day case refers to a patient who receives planned medical and paramedical services delivered in a healthcare facility and who is formally admitted for diagnosis, treatment or other types of healthcare and is discharged on the same day. Day care is the care of a day case.
An in-patient or day care patient is discharged from hospital when formally released after a procedure or course of treatment (episode of care). A discharge may occur because of the finalisation of treatment, signing out against medical advice, transfer to another healthcare institution, or because of death.
The number of deaths from a particular cause of death can be expressed relative to the size of the population. A standardised (rather than crude) death rate can be compiled which is independent of the age and sex structure of a population: this is done as most causes of death vary significantly by age and according to sex and the standardisation facilitates comparisons of rates over time and between countries.
Healthcare resources and activities
Statistics on healthcare resources (such as personnel and medical equipment) and healthcare activities (such as information on surgical operations and procedures and hospital discharges) are documented in this Health in the European Union – facts and figures which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
For hospital discharges and the length of stay in hospitals, the International Shortlist for Hospital Morbidity Tabulation (ISHMT) is used to classify data from 2000 onwards; Chapter IX covers diseases of the circulatory system
hypertensive diseases (0901)
angina pectoris (0902)
acute myocardial infarction (0903)
other ischaemic heart disease (0904)
pulmonary heart disease and diseases of pulmonary circulation (0905)
conduction disorders and cardiac arrhythmias (0906)
heart failure (0907)
cerebrovascular diseases (0908)
atherosclerosis (0909)
varicose veins of lower extremities (0910)
other diseases of the circulatory system (0911)
For surgical operations and procedures, the International Classification of Diseases – clinical modification (ICD-9-CM) is used
operations on the cardiovascular system (35 to 39)
transluminal coronary angioplasty (36.01, 36.02 and 36.05)
bypass anastomosis for heart revascularisation (36.1)
For country specific notes on these data collections, please refer to the annexes at the end of the national metadata reports accessible from links at the beginning of the European metadata report.
The Healthcare non-expenditure statistics manual provides an overview of the classifications, both for mandatory variables and variables provided on a voluntary basis.
Eurostat is in the process of updating the technical requirements for countries to submit hospital discharge data in line with Commission Regulation (EU) 2294/2022. Therefore, the hospital discharge data in this article refer to reference year 2021.
Causes of death
Statistics on causes of death provide information on mortality patterns, supplying information on developments over time in the underlying causes of death. This source is documented in more detail in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions. Under Commission Regulation (EU) 0328/2011 countries provide causes of death data to Eurostat within 24 months (T+24) after the end of the reference year.
Causes of death are classified according to the 86 causes in the European shortlist, which is based on the International Statistical Classification of Diseases and Related Health Problems (ICD). Chapter IX of the ICD covers diseases of the circulatory system
I00 to I02 acute rheumatic fever
I05 to I09 chronic rheumatic heart diseases
I10 to I15 hypertensive diseases
I20 to I25 ischaemic heart diseases
I26 to I28 pulmonary heart disease and diseases of pulmonary circulation
I30 to I52 other forms of heart disease
I60 to I69 cerebrovascular diseases
I70 to I79 diseases of arteries, arterioles and capillaries
I80 to I89 diseases of veins, lymphatic vessels and lymph nodes, not elsewhere classified
I95 to I99 other and unspecified disorders of the circulatory system
Symbols
Tables in this article use the following notation
Value in italics
estimate or provisional data
Value is :
not available
Context
Statistics concerning cardiovascular diseases are of particular significance because these diseases are the principal cause of death within the EU. Increased prevention, especially for heart disease and strokes, has resulted in decreases across most EU countries concerning the number of people who face disability, reduced quality of life and premature death. Nevertheless, cardiovascular diseases continue to touch the lives of millions of Europeans each year.
According to the World Heart Federation, modifiable risk factors for cardiovascular diseases include hypertension, diabetes, obesity, hypercholesterolemia, tobacco and related products use, stress, sleep disorders, sedentary lifestyle, harmful alcohol consumption and unhealthy eating.
Cardiovascular diseases are included as 1 of the 5 main strands covered by the European Commission’s Healthier together – EU non-communicable diseases (NCD) initiative. The initiative was launched in December 2021 and aims to support EU countries in identifying and implementing effective policies and actions to reduce the burden of major NCDs and improve citizens’ health and well-being.
Source link : https://ec.europa.eu/eurostat/statistics-explained/index.php/Cardiovascular_diseases_statistics
Author :
Publish date : 2024-09-16 07:00:00
Copyright for syndicated content belongs to the linked Source.


